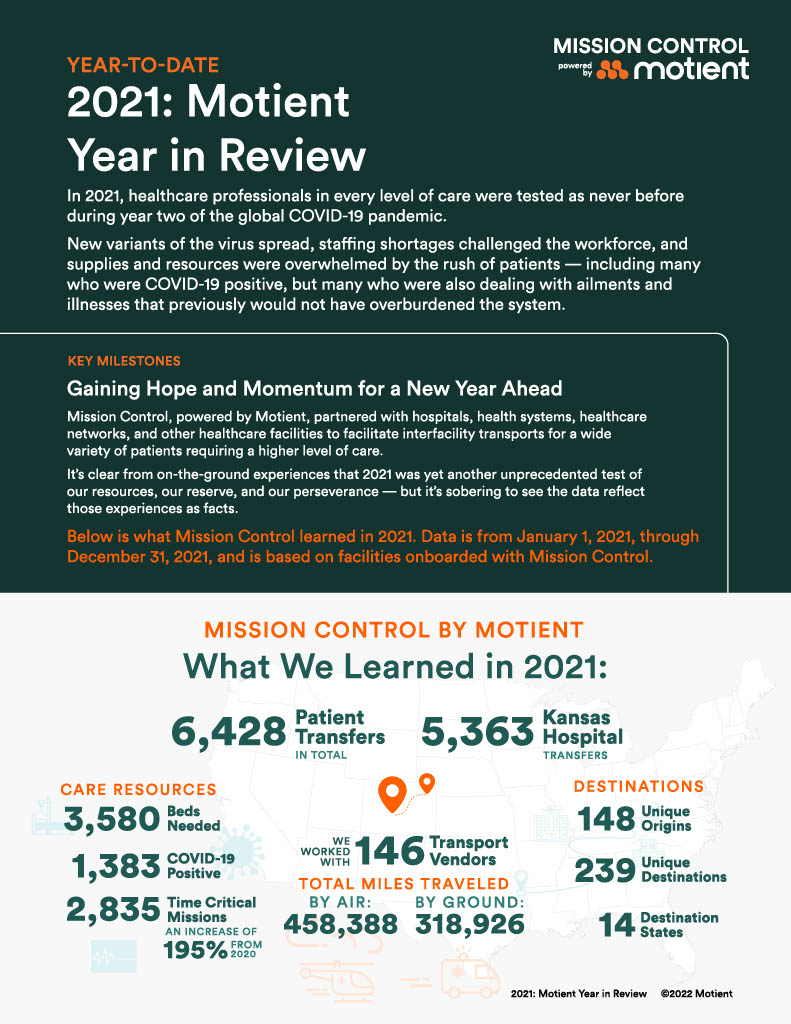
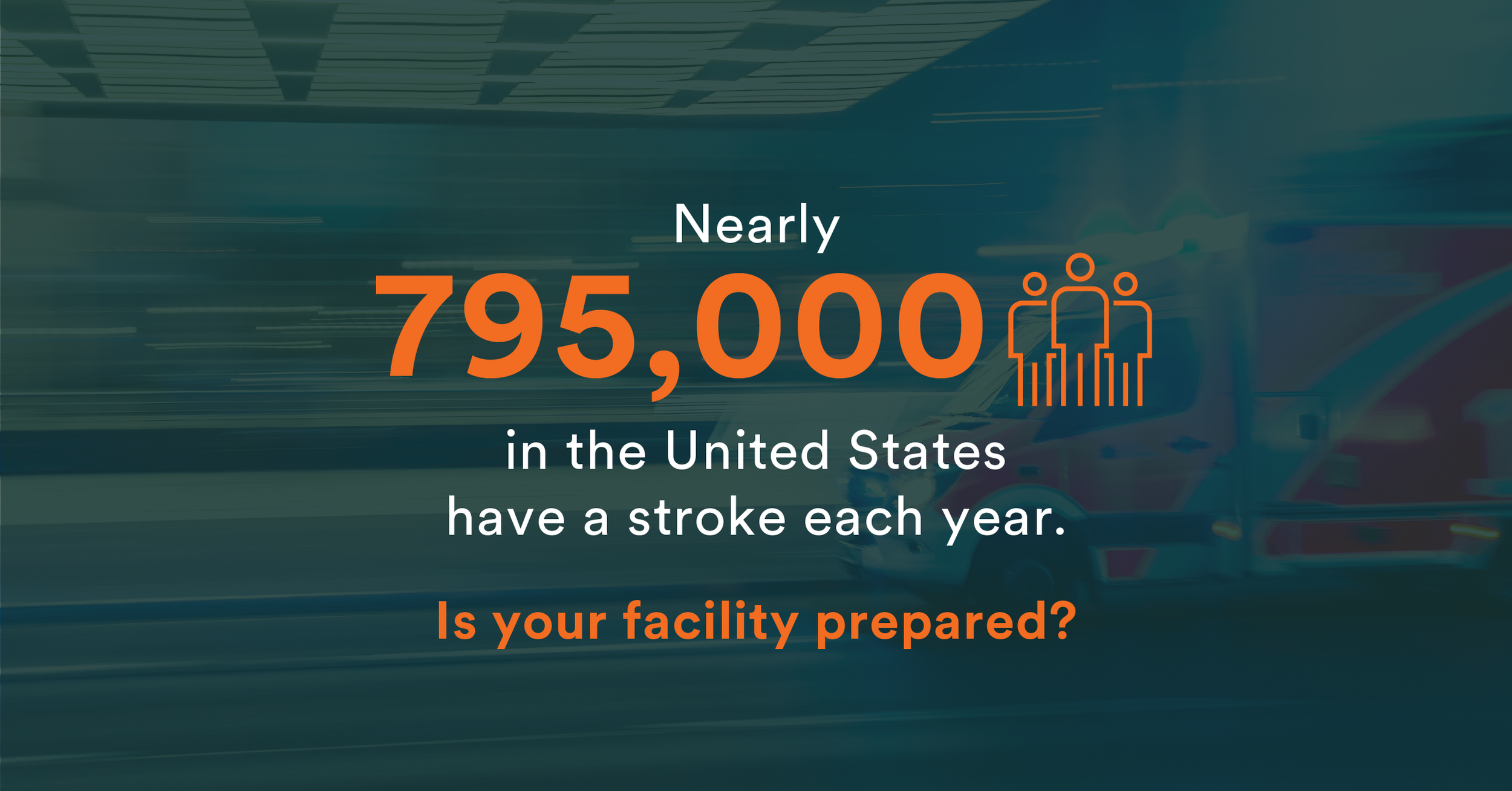
When a patient presents at the ED with signs of a stroke, every second counts. Rapid detection and treatment can increase a patient’s chance of survival and decrease long-term physical and mental complications.
According to a recent study, researchers report that each one-hour treatment delay of a patient with severe stroke correlates with an 11-month loss of “healthy life.” John Hopkins Medicine also outlines how delayed treatment contributes to life-altering conditions like speech and language processing, memory issues, depression, limb weakness, paralysis on one side of the body, and trouble swallowing, depending on the region of the brain affected by the stroke.
Time is of the essence, but expeditiously delivering the appropriate care to stroke patients can be challenging, particularly for America’s rural community and critical access hospitals. These facilities typically don’t have the neurological specialists on staff to assess symptom severity, nor are they equipped to fulfill the care needs of patients suffering from massive stroke. Caring for stroke patients in these settings typically involves stabilizing the patient and getting them to a tertiary facility as quickly as possible. A standardized acuity index and centralized patient movement platform is essential to accelerating this process.
Stroke Assessment and Treatment Protocols
Treating people who experience stroke symptoms requires an enormous amount of medical expertise from physicians. When patients are transferred to a facility by air, in the pre-hospital treatment phase, flight paramedics and registered nurses rely heavily on orders from physicians and nurses at the receiving hospital.
NIH Stroke Scales includes a battery of questions that helps the medical team assess stroke severity. While stroke scales give an initial picture of a person’s physiological symptoms, neurologists need to see brain images to make a full assessment and diagnose stroke.
To treat stroke, thrombolytic medications help dissolve blood clots and restore oxygen flow to the brain.
- TPA tissue plasminogen activator, administered with IV
- Given within three hours of symptom onset [Source: Mayo Clinic]
Click here to read the latest guidelines for early treatment of ischemic stroke, reported by the American Heart Association and American Stroke Association.
During a stroke, getting the patient to the CT is the top priority of the medical team, said Juli Heitman, RN, customer success & quality manager with Motient, Mission Control. She currently works with sending hospital nursing staff who use Mission Control to transfer patients experiencing STEMI, stroke, and sepsis. Previously, Heitman worked as an adult critical care bedside nurse, clinical educator, and quality manager.
Before medications can be administered, Heitman said it is critical to consider several factors that often mimic stroke.
“Before giving a clot-busting drug, first rule out low glucose levels and obtain a completed medication history, especially other blood thinners.”
When monitoring blood pressure during an ischemic stroke, Heitman also said the body will increase the blood pressure to maintain appropriate cerebral perfusion. Lowering the blood pressure too quickly or too much, may cause a further exacerbation of stroke symptoms. [additional source-Critical Care Trauma Centre]
[INFO BOX] Types of Strokes
- Ischemic stroke—indicates limited blood flow to the brain, usually from blood clot
- Transient Ischemic Attack (TIA)
- Hemorrhagic—indicates bleeding on the brain from ruptured artery in the brain
- Posterior stroke–three times more likely of misdiagnosis [Source: CDC and AHA]
Prioritizing Care Means Finding the Best Facility
Prioritizing patient care when a patient shows symptoms of stroke may require interfacility patient transport. And this is especially true for people who live in rural communities with limited resources.
In rural areas, the primary care doctor-to-patient ratio is 39.8 doctors per 100,000 patients compared to 53.3 doctors for the same patient load in urban settings, according to National Rural Health Association. And the number of specialists like cardiologists and neurologists–even lower in rural areas.
Do you have the right tools to make quick decisions about patient transfers? Let’s face it, there are many moving parts when it comes to sending patients to and from facilities. While planning and coordinating these efforts, it’s just as important to maintain high-quality patient care. At Motient, we believe Mission Control can help with both.
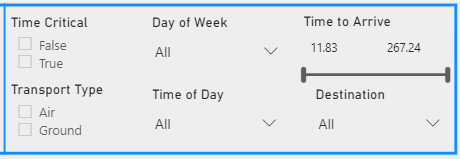
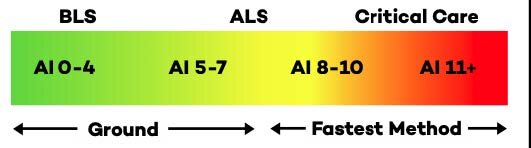
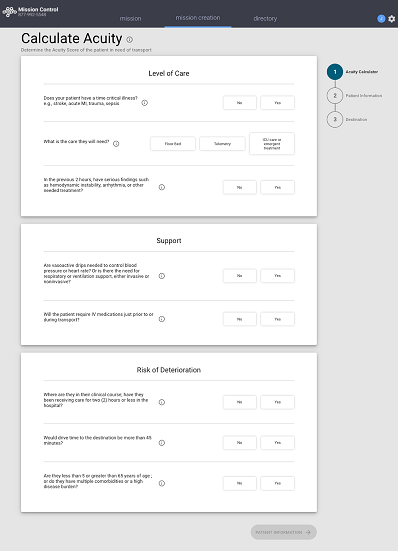
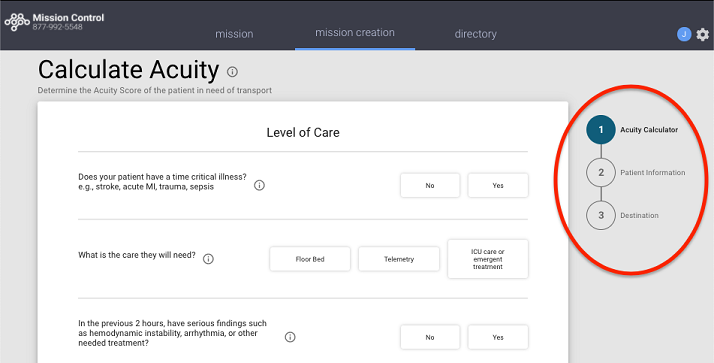
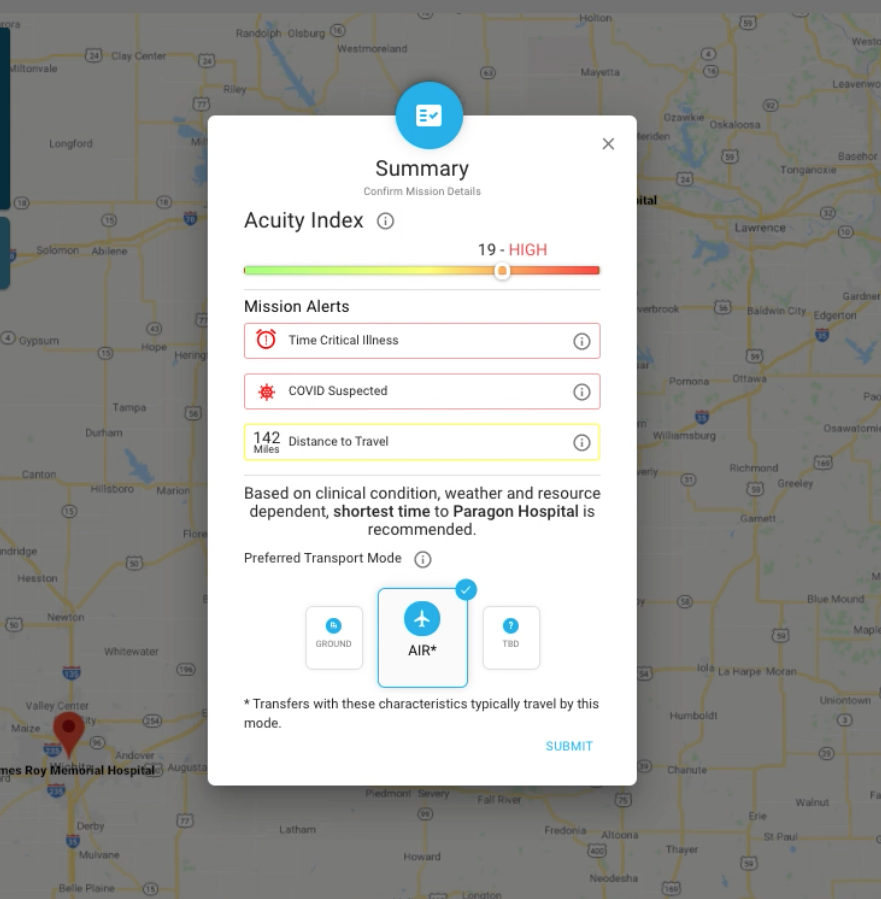
To conduct safe, efficient patient transfers, having access to tools like the Acuity Index built into Mission Control can make all the difference. Think of the Acuity Index as a common language that helps clinicians assess patient severity and monitor worsening conditions while deciding the best method of transport, whether by air or ground.
When a patient rapidly deteriorates and needs an urgent transfer, Mission Control also helps ease the search of finding a receiving facility with beds. That means sending facilities can expedite transfers so that patients receive time sensitive quality care from receiving facilities.
“Our goal is to supply the information and structure so facilities and hospital systems can make informed choices about moving patients from one place to another,” Richard Watson, MD, Motient co-founder said, during a podcast interview with “An Empowered Patient.”
How Mission Control Helps the Healthcare Team
- Facilitates early activation of resources and IFT
- Reduces door to needle time – ideal goal 90 minutes
- GPS tracking—real time tracking from the sky
Want to learn more about how Mission Control can help your facility ease the coordination of patient transfers while maintaining high-quality patient care? Visit Motient.io and request a demo today.
Taking a standardized approach to acuity assessments not only provides more objectivity, but also gives hospitals the data they need to make a variety of tactical and strategic decisions, from daily unit staffing to future space, specialty services, and bed capacity.
In addition to providing clinicians with a standardized perspective of their patient populations, acuity assessments also enhance patient safety. The number of handoffs between inpatient care providers and units is a proven risk factor for negative clinical outcomes, and a uniform language of assessment can help manage that risk.
The decision to transfer a patient to another facility reflects a myriad of considerations. Unlike much of medicine, the decision is traditionally made without the benefit of a large body of evidence. In the emergency department, a patient’s care is driven by the experience of physicians, nurses, and ancillary staff, who rely on their accumulated clinical wisdom in selecting the next step in a patient’s care. Yet when a patient is handed off to a transport team for transfer, there is often a communication gap regarding how the patient’s current condition, their care needs during transport and upon arrival, and the risk of those needs changing.
Although patient handoffs are central to the field of medical transport, there are no national standards for patient severity of illness, or the clinician accreditation needed for that severity. According to the Association of Critical Care Transport, a national patient advocacy association, this lack of standardization presents patient safety risks that are often invisible to referring and receiving clinicians, as well as to patients and their families.
Transport staff delivering a patient to the hospital or another care setting initially seek to understand two variables: exactly how sick the patient is, and how urgently they need the care at their destination. A standardized communication framework that centers on patient acuity and uses objective language turns this universal assessment into a repeatable, organized process that can be applied to every patient across the board.
The patient’s acuity functions as the most pivotal information at a fundamental point-of-care decision point: do we have the resources to give this patient what they need, or will they require greater resources available at another facility? An acuity score allows sending and receiving hospitals to prioritize patient movement based on the time-sensitive acuity of those patients. Receiving centers can also survey incoming patients to assist in their internal bed management.
When clinicians have the common language of acuity at their disposal, the patient’s score functions as shorthand, immediately conveying the difference between patients. This utility is essential, as a score can quickly communicate the core gestalt of “how sick is this patient?” without the listener having to parse the details in that moment.