The ins and outs of interfacility patient transports — the processes, workflows, resources, reimbursement, and decision-making — aren’t something most people think about.
Yet how patients move within a healthcare system impacts not only the patient being transferred, but also the transport vendor and the on-call physician, as well as the hospital’s program director, board members, and local and state stakeholders. How patients move influences much more than most people think, and its impact can be seen on the national level as we look at our healthcare statistics and trends. Let’s learn a little more.
A Patient Arrives at the Emergency Room (ED)
When a patient arrives at the ED, a triage nurse assesses the severity of their condition based on vital signs, symptoms, and medical history. After triage, a physician must determine the individual’s subsequent needs: does the facility have the expertise, resources, and equipment to treat this patient? If not, the ED team might initiate an interfacility transfer.
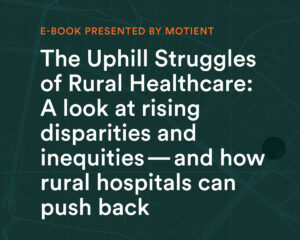
Approximately 70% of a hospital’s inpatients are processed in through the ED, and the majority arrive by Emergency Medical Services (EMS). For the most urgent conditions — such as myocardial infarction, stroke, sepsis, and major trauma — EMS protocols specify emergent transport to the most appropriate facility for immediate treatment. But once these patients are stabilized, they might still require a transfer.
Patients often qualify for an emergent transfer to another facility because their condition requires a level of specialization or testing that the initial facility cannot offer. For example, a trauma patient who requires surgery might be transferred from a critical access hospital (one with 25 or fewer acute care beds) to a Level I trauma center. Before the COVID-19 pandemic, smaller EDs averaged the highest transfer rates, at approximately 5%.
Patients can also be transferred due to a lack of capacity (which is happening much more frequently during our current staffing crisis), patient preference, or insurance coverage issues. In non-emergent situations, a patient might require transfer for elective surgery, to be closer to home, or to move to a more suitable environment in order to free up capacity for high-acuity patients.
The Patient Needs to Be Transferred
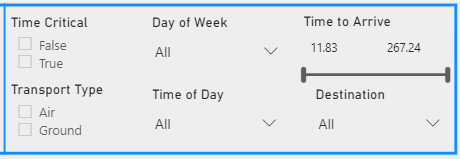
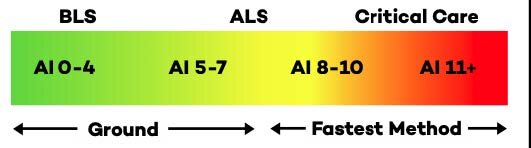
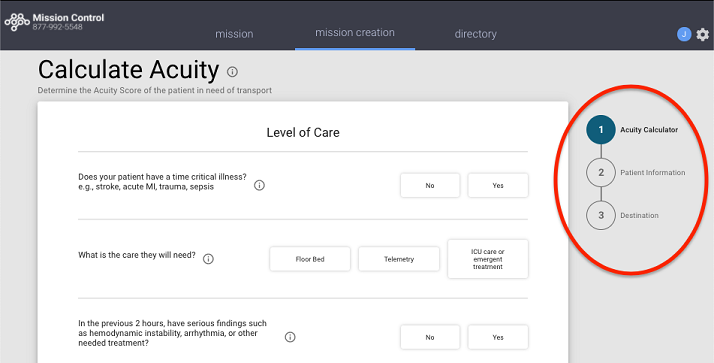
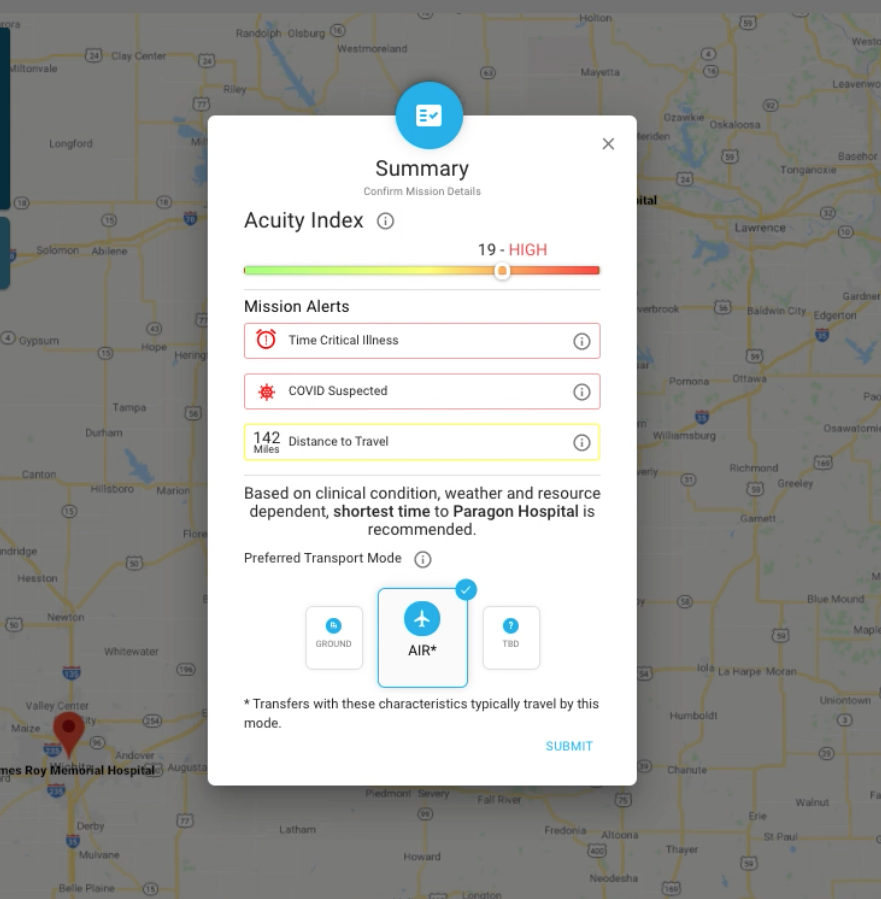
Time-critical cases require fast consideration of the patient’s clinical situation, current needs, potential outcomes, and the available resources. Facilities must have standardized processes in place to quickly evaluate their capacity for accommodating a patient who requires a higher level of care. Hospitals can use acuity scores to prioritize which patients should be first on the list for a transfer, ensuring that low-acuity cases do not inadvertently bump higher-acuity cases down the list.
Hospitals must also have strong connections with other hospitals within the region, as they will need to locate and confirm an appropriate destination. When bed capacity drops across a region — such as during COVID-19 — finding a facility that can receive the patient can be a challenge. Clinicians sometimes spend hours on the phone, calling half a dozen facilities or more in search of a bed. For facilities using Motient’s Mission Control solution, the process is much easier. Clinicians simply enter a pending transfer into the application and continue caring for patients, as the Motient team will contact them once an appropriate, available destination is confirmed.
What kind of prep work must be done?
Once an appropriate placement is found, the ED team must coordinate the logistics of safe, reliable patient transport. The team may need to contact multiple transport vendors, as some may be unavailable, or may lack the capabilities for safe transport for certain patients. An incomplete understanding of the patient’s condition can lead to inadequate resources during transport, and thus to adverse events.
Throughout the transfer process, physicians at both the referring and receiving hospitals must be updated about any changes in the patient’s status. There should be open and continual communication between the medical command and the transporting vehicle. The key elements of a safe interfacility transfer include communicating the transfer decision; stabilizing and preparing the patient; choosing the appropriate means of transport; determining the degree of monitoring required during transport; and ensuring a smooth patient handover to the receiving facility. While Motient’s Mission Control solution provides essential support for all of these functions, hospitals without a patient transport tool may struggle to manage the logistics of the transfer process on their own.
Why is a standardized infrastructure necessary?
As the pandemic has shown us, patients who spend too much time in the wrong level of care have a ripple effect across healthcare, impacting the number of beds available for high-acuity patients. Ideally, hospitals and other healthcare facilities should be able to access regional patient transport data to give them insight into capacity blockages, available specialty resources, and ongoing needs.
Hospitals that establish an overarching process for how they will handle interfacility transfers will be better equipped to make fast, efficient choices to reduce risks and maintain care quality. By specifying best practices for certain clinical conditions, patient circumstances, and system and staffing constraints, hospitals can conserve limited resources and deliver patients to the best possible care setting.

More and more hospitals are beginning to collaborate with their regional counterparts to develop a better infrastructure for patient movement. For example, larger academic medical centers might agree to receiving patients from urgent care centers and rural hospitals, while smaller hospitals might commit to receiving lower-acuity patients plus a particular subspecialty. When hospitals work together, they can better ensure that all patients receive the care they need without blocking movement within the larger ecosystem.
While regional collaboration was important before COVID-19, it is now essential. Motient’s Mission Control gives hospitals the tools they need to streamline the transfer process. As hospitals refine their own patient movement performance, they will be better equipped to partner with other facilities to establish a regional transfer infrastructure—one that ensures every patient is treated in the best possible location for his or her condition.
To learn more, read this article by Motient co-founder Martin Sellberg, MD, FACEP, How Patient Movement Benefits from Standardized Acuity Scoring in HIT Consultant.