A patient assessment score helps health care teams allocate resources and determine the appropriate care a person should receive. Until now, there has been no standardized methodology to determine the vital, transfer-specific elements of a person’s condition as necessary to how they will be moved between facilities, using which modalities and resources.
Founded in Decades of Real-World Expertise
The Acuity Index was created by Martin Sellberg, M.D., FACEP, and contributed to by Richard Watson, M.D. It’s based on their combined decades of emergency medicine and medical transport experience in various emergency departments, from rural and frontier settings to major urban trauma centers.
Drs. Sellberg and Watson recognized a need to assess the unique variables considered during adult interfacility transfers. When a person is removed from the resource-rich environment of a hospital or similar setting, there must be a commonly understood measurement to determine their current and continued stability, the interventions and monitoring skills needed to maintain that stability, and their risk of deterioration once they leave the hospital and begin their journey to definitive care.
The Acuity Index helps answer questions like this: What do providers consider when determining the most appropriate mode of transport for a patient who needs a neurological intervention 90 miles away versus a stable orthopedic injured patient at the same facility when their receiving hospital is 200 miles away?
8 Questions. 3 Key Areas. Invaluable Information.
The Acuity Index asks healthcare professionals to answer eight questions. The questions consider clinical workload, risk, a prognostic perspective of the patient, and in general, the level of care needed based on the severity of illness, all critical components of moving the patient between controlled and uncontrolled environments.

These eight questions are broken into three parts that determine patient level of care, support, and risk of deterioration.
1. Level of care and monitoring the patient will receive at the destination facility
2. Physiological support or intervention needed to maintain patient stability
3. Risk of deterioration during transfer
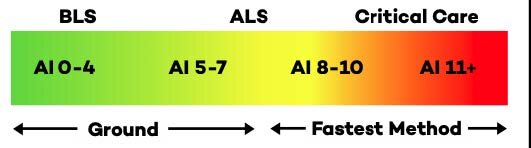
The information gathered under these categories is weighted and assigns a numerical value to the person being assessed. The value reflects the patient’s illness level or severity to help determine the level of care needed in the transfer process, such as crew capability, recommended mode, and other factors — information that was previously not possible to standardize. This Acuity Score stratifies patients into groupings to aid quality departments and enhance reporting processes.
The Acuity Index Creates a Common Language for Interfacility Transfer Assessment
The Acuity Index creates a common language for transfer assessment. Instead of increasing the saturation of assessment scores, however, the Acuity Index fills a critical need: The value of the Acuity Index is specific to patient movement, an assessment that previously did not exist.
The decisions made regarding destination and timing, and mode and level of care, in patient movement have far-reaching effects on financial and clinical outcomes. Healthcare cannot afford transport decision-making based on random or incomplete information, and the strategy, “this is the way we’ve always done it,” makes little business sense. Instead, interfacility transport should be guided by an organized assessment and decision process and data that can be shared through the system to assist in further dialogue to identify and solve local challenges collaboratively. The Acuity Index explicitly scores a person’s condition as appropriate for critical transport points between the sender, EMS, and the receiver. It has a specific use and value applied directly to patient movement.

The Acuity Index also creates significant value in enabling patient stratification for transfer reporting and quality metrics. The Acuity Score enables quality managers to evaluate resource utilization across patient types, DRGs, and Acuity Scores. Furthermore, the Acuity Score can be used for reimbursement justification and Time Critical Diagnosis assessment and reporting.
Please contact us here to learn more about the Acuity Index and Mission Control.


